健康・医療Measles
- 日本語
- English
What is measles?
Measles is known as an acute systemic infectious disease caused by measles virus.
It is spread by air-borne, droplet and contact infection, and transmitted from human to human and is highly contagious. When people who have no immunity are infected, they will develop the symptomatic disease almost 100% of the time. Once infected and having developed the symptomatic disease, they will continue to be immune throughout their life.
Occurrences
Measles becomes epidemic from spring to early summer every year. Looking at the past trends, there was an outbreak mostly among people in their 10s and 20s from 2007 to 2008. However, opportunities for a second dose of measles vaccine for people at the age of seventh grader and high-school senior for the five years since 2008 and other measures drastically decreased the number of patients in their 10s and 20s since 2009. The largest patient group is 0 to 1 year-olds while the rate of cases of adults aged 20 or above is also increasing.
Viral isolations and detections since November 2010 found that there have been only cases with imported viruses and there are no cases due to the genotype D5 that caused the epidemic in Japan from 2007 to 2008.
On March 27, 2015, the World Health Organization Western Pacific Regional Office verified that Japan had achieved measles elimination. However, there have been outbreaks spreading from imported case. The latest number of reported cases based on infection surveillance of measles is regularly posted on the website of the National Institute of Infectious Diseases (NIID). Information on measles can be confirmed on the website of the NIID Infectious Disease Surveillance Center.
Viral isolations and detections since November 2010 found that there have been only cases with imported viruses and there are no cases due to the genotype D5 that caused the epidemic in Japan from 2007 to 2008.
On March 27, 2015, the World Health Organization Western Pacific Regional Office verified that Japan had achieved measles elimination. However, there have been outbreaks spreading from imported case. The latest number of reported cases based on infection surveillance of measles is regularly posted on the website of the National Institute of Infectious Diseases (NIID). Information on measles can be confirmed on the website of the NIID Infectious Disease Surveillance Center.
If you have the measles
About 10 days after infection, cold-like symptoms such as fever, cough and a runny nose occur. The fever persists for two to three days before developing a high fever over 39 C with a rash. Measles patients often develops compilications such as severe respiratory infections (e.g. pneumonia) and ear infections (e.g. otitis media). It is said that one of 1,000 measles patients develops encephalitis. Furthermore, one of 1000 patients die even in developed countries.
Other complications with measles include a central nervous system disease called subacute sclerosing panencephalitis (SSPE) especially among school age children though its occurrence is rare (one of 100,000 patients.) In recent years, two doses of measles-containing vaccine are given and the number of measles cases is subsequently decreasing.
Other complications with measles include a central nervous system disease called subacute sclerosing panencephalitis (SSPE) especially among school age children though its occurrence is rare (one of 100,000 patients.) In recent years, two doses of measles-containing vaccine are given and the number of measles cases is subsequently decreasing.
Vaccine
Measles is highly contagious and spread through the air. Therefore, washing hands and wearing a mask are insufficient to prevent infection, and measles vaccination is the most effective measure. It is also considered effective to receive measles vaccination within 72 hours of initial measles exposure. Gamma globulin injection within five to six days after exposure may suppress developing the disease, but this is not an option to choose easily. For the details, consult your primary care physician. Not only people eligible for routine immunization but also medical/educational personnel and adults planning traveling abroad are recommended to consider measles vaccination if the past medical history of measles or vaccination history is uncertain.
It is said that more than 95% of people who have received a measles-containing vaccine (mostly measles-rubella vaccine) acquire immunity against measles. Second vaccination gives immunity to many of those who failed to acquire immunity by the first dose. For people whose immunity weakened over time after vaccination, the second dose is effective to reinforce their immunity. Since FY2006, children have received measle-containing vaccine twice, when they are one-year old and during the year prior to admission to elementary school. In addition, the second dose of vaccination had been introduced as routine immunization for people at the age of seventh grader and high-school senior for the five years from FY2008 to FY2012.
The most common reaction to the first vaccination is fever. It occurs most frequently around one week after vaccination but about 13% of vaccinated people develop fever within two weeks after the shot. Several percent of vaccinated people develop a rash around one week after the shot. About 3% get hives as allergic reaction while about 0.3% could cause a febrile convulsion. The second dose may cause local reaction on the injection part but the frequency of developing fever and rash is very low. In addition, encephalitis/encephalopathy is one of the rare side effects reported at the frequency of lower than one out of 1 to 1.5 million, which includes cases without clear causal relationship. Measles-containing vaccine is produced using germ cells of chicken. Because an egg itself is not used, it is thought to be safe from allergic reaction to eggs. However, if you are seriously allergic (experiencing anaphylactic reaction in the past, for example), consult your primary care physician before receiving vaccination because other conponents of vaccine product could cause an allergic reaction.
See here for the implementation status of vaccination
It is said that more than 95% of people who have received a measles-containing vaccine (mostly measles-rubella vaccine) acquire immunity against measles. Second vaccination gives immunity to many of those who failed to acquire immunity by the first dose. For people whose immunity weakened over time after vaccination, the second dose is effective to reinforce their immunity. Since FY2006, children have received measle-containing vaccine twice, when they are one-year old and during the year prior to admission to elementary school. In addition, the second dose of vaccination had been introduced as routine immunization for people at the age of seventh grader and high-school senior for the five years from FY2008 to FY2012.
The most common reaction to the first vaccination is fever. It occurs most frequently around one week after vaccination but about 13% of vaccinated people develop fever within two weeks after the shot. Several percent of vaccinated people develop a rash around one week after the shot. About 3% get hives as allergic reaction while about 0.3% could cause a febrile convulsion. The second dose may cause local reaction on the injection part but the frequency of developing fever and rash is very low. In addition, encephalitis/encephalopathy is one of the rare side effects reported at the frequency of lower than one out of 1 to 1.5 million, which includes cases without clear causal relationship. Measles-containing vaccine is produced using germ cells of chicken. Because an egg itself is not used, it is thought to be safe from allergic reaction to eggs. However, if you are seriously allergic (experiencing anaphylactic reaction in the past, for example), consult your primary care physician before receiving vaccination because other conponents of vaccine product could cause an allergic reaction.
See here for the implementation status of vaccination
Q&A
- Q1.Why did measles become epidemic mostly among people in their 10s and 20s from 2007 to 2008?
- A1. It was common to be infected with measles and naturally acquire immunity during childhood. The increased measles vaccination coverage, however, decreased the number of measles cases. Some people in their 10s and 20s have not received measles vaccination. In addition, a single dose of vaccination does not always confer sufficient immunity. It is known that a small percent of people do not acquire sufficient immunity by receiving measles vaccination just once. It is believed that such people were one of the causes of the epidemic.
Furthermore, the increased coverage of measles vaccination decreased the number of measles patients, which decreased opportunities for exposure to measles virus. As a result, people in their 10s and 20s at the time who had received measles vaccination only once in their childhood could not reinforce their immunity, which gradually weakened over time. This is also believed to be another cause of the epidemic. - Q2.I am pregnant and worried about measles epidemic. What can I do?
- A2.Getting infected with measles during pregnancy has potential to cause miscarriage or premature birth. Women who have not received a measles-containing vaccine or contracted the disease should actively consider receiving the vaccine before pregnancy. However, women known to be pregnant should not receive measles vaccine in general. You need to stay indoors and avoid crowds during measles epidemic. If your housemate is likely to contract measles (e.g. healthcare professionals and educators who have not completed two doses of measles vaccination and are more likely to be exposed to measles virus) during measles epidemic, consult your physician about vaccination and other measures.
- Q3.Does contracting measles overseas cause a lot of trouble?
- A3.If you develop measles in countries/regions where there are either none or only rare measles cases, not only you but also your traveling companion will be strictly restricted in travelling for the purpose of preventing spread of the infection.
- Q4.Is there anything that needs special attention concerning measles when traveling abroad?
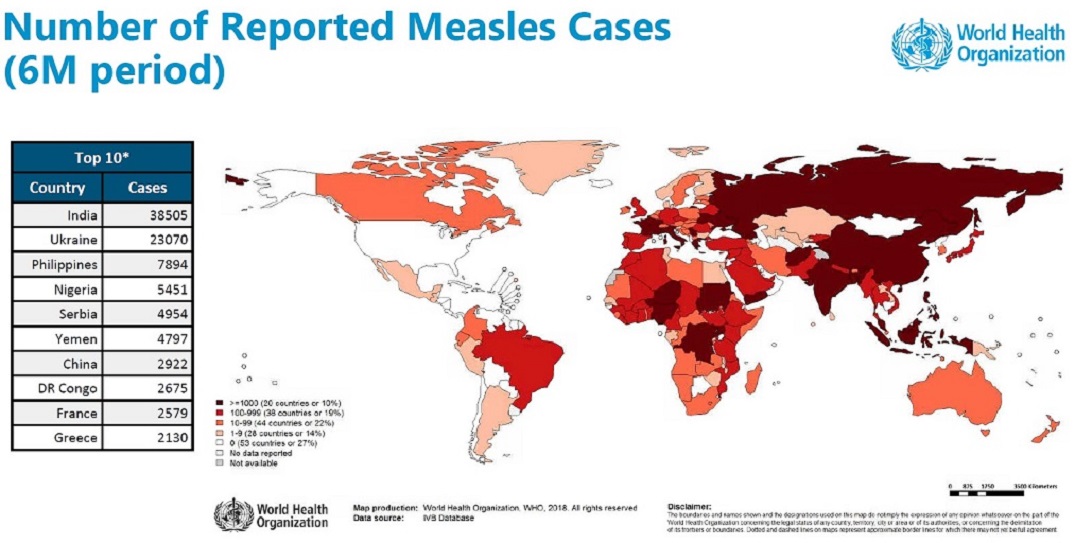
- A4.. Only from a few to double digit measles cases are reported annually in Americas (imported cases and those related to them) and many Middle Eastern and European countries. On March 2015, the World Health Organization (WHO) Western Pacific Regional Office verified that Japan had achieved measles elimination. On the other hand, still a large number of patients are reported in Asian and African countries. There are many reported cases especially from China, India, Mongolia, Pakistan, Nigeria and other countries shown in brown color in the map below.
Most developed countries including Japan have adopted two doses of measles-containing vaccination (mostly MMR (measles, mumps and rubella) vaccine) against measles. Accordingly there are an increasing number of countries achieving measles elimination. On September 27, 2016, WHO declared that the Region of the Americas had eliminated measles.
However, there are still many measles cases (diagnosed through examination) in many regions as shown by the figure below. Therefore, we recommend people who have not contracted (been diagnosed with) measles to check their measles vaccination history before traveling overseas, and, if they have not received two doses of vaccination or past vaccination history is unknown or uncertain, to receive measles vaccination.
- Quarantine Information Office, Ministry of Health, Labour and Welfare, the Government of Japan (FORTH) measles/rubella epidemic situation (as of April 2016)
- Fact sheet (Measles) Original text(WHO)(in English)
- Tabiregi (Ministry of Foreign Affairs)
- WHO Immunization Data portal - All Data
- Q5.I have had measles in the past. Should I receive measles vaccination?
- A5.If it is definite that you have had measles in the past (measles infection was confirmed through examination), you are immune to measles and do not need to receive vaccination. If it is uncertain whether you have had measles, consult your physician. Vaccination to people with a history of measles will not increase adverse effects.
Even if you have had either measles or rubella, you can receive measles-rubella vaccine as routine immunization if you are eligible age for the routine immunization. - Q6.Who is recommended to be vaccinated?
- A6. People in the target age of routine immunization (infants in their second year of life and children in the year prior to admission to elementary school) are subject to active recommendation. Others who have never contracted measles or been vaccinated are recommended to consult their primary care physician.
People who were born on April 2, 1990 or later receive two doses of measles-containing vaccine as routine immunization, but most people who were born before the date have received only one dose. Especially healthcare, school, nursing/welfare personnel and other people at increased risk of measles or who will have a large impact on people around them by contracting measles, and people who plan to travel overseas are recommended to consult their physician regarding the second dose of vaccination. - Q7.Is there any health problem in receiving MR vaccine (measles-rubella vaccine) instead of measles vaccine alone as preventive vaccination against measles?
- A7.MR vaccine is expected to have measles prevention effect similar to a measles monovalent vaccine.
There is no health problem in receiving MR vaccine instead of measles monovalent vaccine. It has an advantage of preventing also rubella.
However, because MR vaccine is live attenuated vaccine, women known to be pregnant should not receive it. Even if you are currently not pregnant, pregnancy should be avoided for about two months following MR vaccine to avoid influence on the fetus as much as possible.
Women known to be pregnant should not receive monovalent measles vaccine or rubella vaccine either. It is also necessary to avoid pregnancy for about two months following vaccination and take similar precautions.
Reference data for traveling overseas
Figure: Number of reported measles cases by country (from September 2017 to February 2018)